ICE activity in and around hospitals is creating fear that deters patients and staff from seeking or providing care. DHS’s rescission of the "protected areas" policy has amplified concerns that hospitals are no longer safe havens. Health workers report workplace anxiety and subpoenas for employment documents, while medical groups warn that fear-driven delays worsen health outcomes and strain emergency services.
I’m a Doctor: ICE Presence at Hospitals Is Driving Patients Away and Harming Care

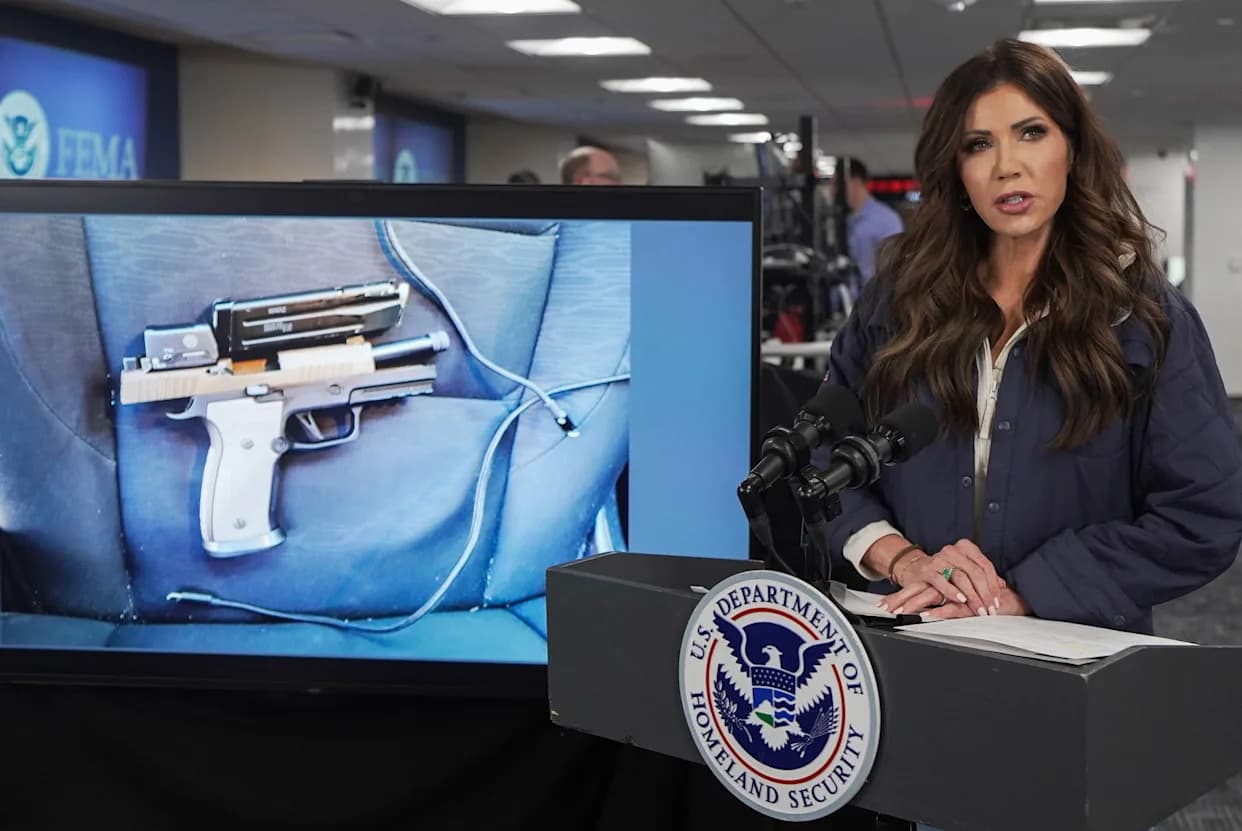
In July, a Salvadoran woman detained by Immigration and Customs Enforcement (ICE) experienced a medical emergency while in custody. Her attorney says ICE escorted her to a Los Angeles–area hospital, where agents reportedly waited in the lobby around the clock for two weeks. She was later moved to another facility where agents allegedly positioned themselves inside her room and pressured her to say she was well enough to be discharged.
Fear Inside Health-Care Spaces
The visible presence of immigration agents in and around hospitals and clinics is creating widespread fear among patients, families and health-care staff. Last year the Department of Homeland Security rescinded its long-standing "protected areas" policy that had limited immigration enforcement at schools, hospitals and houses of worship. That policy change signaled that places once treated as off-limits may no longer be safe from enforcement actions.
Across the country, this perceived loss of safety is changing behavior. An AKFF/New York Times survey of immigrant communities published in November found that heightened enforcement has generated deep anxiety and uncertainty, making many people less willing to enroll in health coverage or to seek medical care.
Not Just Undocumented People Are Affected
Fear extends beyond people without legal status. Janell Johnson Thiele, a nurse at Hennepin County Medical Center in Minneapolis, told MedPage Today that some U.S. citizens have become reluctant to seek care because they speak with an accent or fear being profiled by appearance. Staff anxiety is also rising: DHS issued a subpoena on Jan. 8 to Hennepin Healthcare for its I-9 employment forms, and workers have reported seeing ICE in hospital buildings and feeling afraid to come to work.
“When people are afraid to seek medical attention for themselves or their families, it threatens their health, impedes the ability of physicians to render care, and ultimately undermines basic trust in our health care institutions.” — American Medical Association
The AMA issued this statement in response to reports of enforcement activity near emergency rooms and hospitals, warning that such actions create systemic risks to patient care and public health.
Consequences For Health And Systems
From the Deep South to the Pacific Northwest, clinicians report that immigrants are delaying or avoiding care to reduce the risk of detention. In Portland, Oregon, a nurses' union warned that ICE officers pressured clinicians to skip assessments and monitoring so detainees could be discharged faster. Fear erodes attention, judgment and teamwork, increases burnout and absenteeism, and ultimately compromises care for all patients.
Delaying routine care has measurable consequences: missed medications lead to complications, untreated infections can spread and worsen, and delayed prenatal care raises maternal and infant risks. As an emergency physician, I have repeatedly seen conditions that could have been managed in clinic settings become urgent crises by the time patients present to the emergency department. That shifts the burden to already strained acute-care systems.
Why People Choose Not To Seek Care
For many patients the decision is practical, not political. They ask: Will coming to the hospital make me more vulnerable? Could I be questioned or detained? If I am detained, will my family be able to find me? Some hospitals are accused of using so-called "blackout" procedures — registering people in custody under pseudonyms and declining to confirm their location to relatives — which only increases fear and uncertainty.
When answers are uncertain, waiting often feels safer than seeking help. Families weigh urgent medical needs against the risk of separation, and this calculus widens health disparities across communities—affecting not only undocumented immigrants but anyone perceived as "out of place."
What’s at Stake
Immigration enforcement in and near medical facilities is more than an immigration-policy debate. It is a public-health problem that undermines trust in institutions designed to protect and heal. When hospitals stop feeling safe, patients delay care, health systems strain, and preventable complications rise—putting everyone at greater risk.
Help us improve.