Researchers transplanted fecal microbiota from people in a depressive phase of bipolar disorder into mice and observed depression-like behavior and reduced synaptic connectivity in the medial prefrontal cortex. Animals receiving microbiota from healthy donors did not show these changes. Fluoxetine had no effect, while lithium restored normal behavior—paralleling clinical treatment patterns. The transplanted samples contained bacteria such as Klebsiella and Alistipes, though researchers stress microbes are likely one of multiple contributing factors. The study appears in Molecular Psychiatry.
Gut Microbes Alter Brain Wiring and Drive Bipolar-Like Depression in Mice, Study Finds

A new animal study from Zhejiang University suggests that specific imbalances in gut bacteria can change neuronal connectivity and produce depressive symptoms resembling bipolar depression.
Researchers transplanted fecal microbiota from human volunteers—each confirmed to be in a depressive phase of bipolar disorder within the previous 24 hours—into healthy mice. Using brain imaging, genetic sequencing and behavioral assays, the team found that recipient mice developed depression-like behaviors, including reduced movement and diminished interest in rewarding treats (anhedonia).
Importantly, the investigators observed weakened synaptic connectivity in the medial prefrontal cortex (mPFC), a brain region involved in decision-making and emotional regulation, and disruption of reward-related circuits. Animals that received microbiota from healthy donors did not show these neural or behavioral changes.
"Mice transplanted with fecal microbiota from bipolar disorder patients displayed bipolar disorder depression-like behavior, accompanied by changes in neural structure and synaptic connectivity in the mPFC," the authors report.
To probe the nature of this depressive phenotype, the team tested two medications: fluoxetine (a common antidepressant) and lithium (a first-line mood stabilizer for bipolar disorder). Fluoxetine produced no measurable benefit in the affected mice, whereas lithium substantially restored normal activity and interest—mirroring clinical differences in how bipolar depression often responds to treatment.
Microbial profiling of the transplanted samples identified genera previously linked to negative mental-health outcomes, including Klebsiella and Alistipes. The authors caution that while these taxa were associated with the observed changes, additional work is needed to establish direct causal roles and mechanisms.

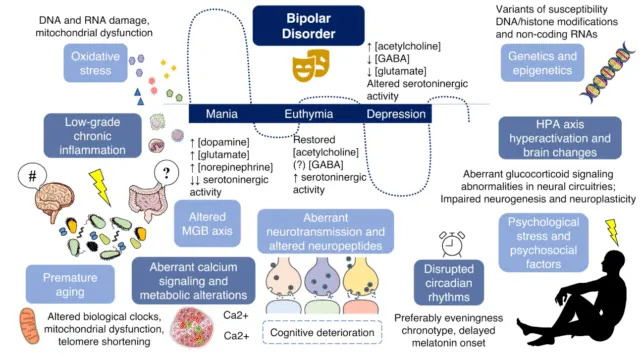
The researchers emphasize that bipolar disorder is multifactorial—driven by genetic, environmental and lifestyle influences—and that gut microbes are unlikely to be the sole cause. Instead, microbiome alterations may be one contributing layer that increases vulnerability or worsens symptoms.
Implications and Next Steps
These findings strengthen the link between the gut microbiome and brain function and raise the possibility that restoring healthy microbial communities could become a therapeutic strategy to reduce depressive symptoms in bipolar disorder. However, translation to humans will require careful clinical studies to identify precise microbial targets and confirm safety and efficacy.
The full study is published in Molecular Psychiatry.
Help us improve.


































