New research in mice shows that untreated obstructive sleep apnoea — which causes repeated drops in blood oxygen during sleep — can accelerate heart ageing and raise mortality risk. Mice exposed to intermittent hypoxia had higher death rates and developed high blood pressure, impaired cardiac function, vascular stiffening and ECG abnormalities. The study underscores the need for early diagnosis and treatment, including CPAP, while noting results come from an animal model and require cautious translation to humans.
Untreated Sleep Apnoea May Speed Heart Ageing And Raise Early-Death Risk, Study Finds

Leaving obstructive sleep apnoea untreated may accelerate the biological ageing of the heart and increase the risk of premature death, new research in a mouse model suggests. The study links repeated drops in blood oxygen during sleep to lasting damage to cardiovascular structure and function.
What Is Sleep Apnoea?
Obstructive sleep apnoea is a common breathing disorder that occurs during sleep and causes repeated pauses or irregularities in breathing. Episodes can last from a few seconds to minutes and often lead to daytime sleepiness, loud snoring and persistent fatigue despite adequate time in bed.
The Study And Key Findings
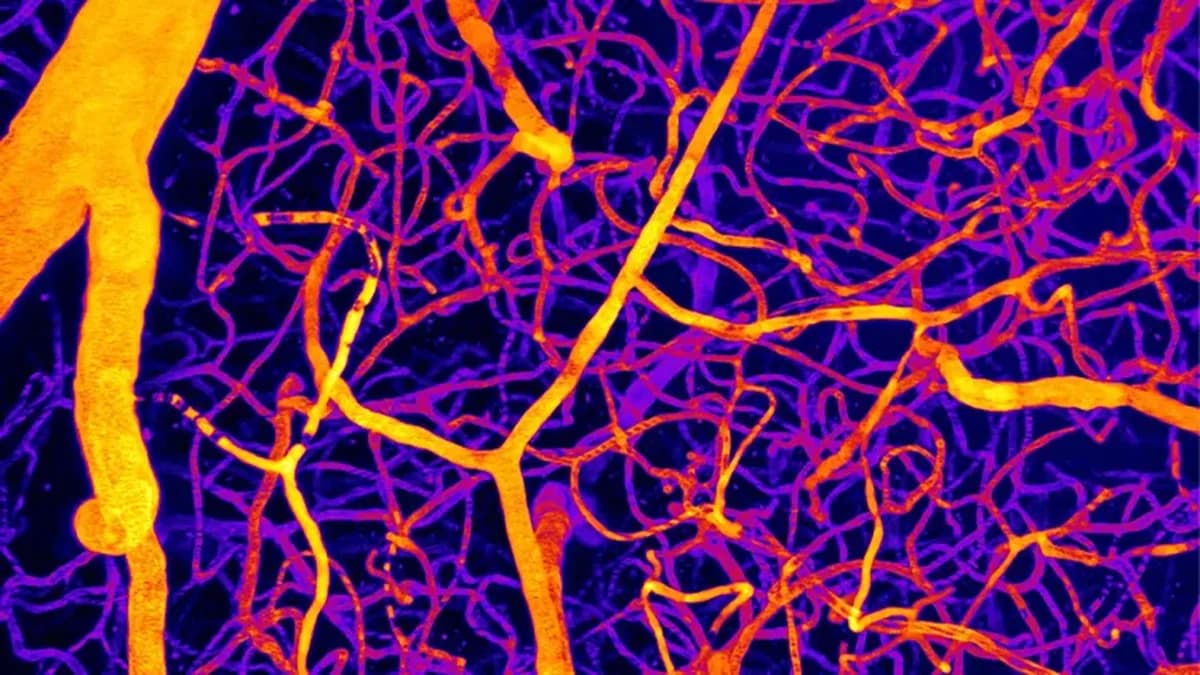
Researchers used a specialised mouse model to mimic the intermittent falls in blood oxygen — called intermittent hypoxia — that characterise obstructive sleep apnoea. They followed animals throughout their lifespans to assess how chronic exposure to fluctuating oxygen levels affected heart health.
Compared with control animals kept under normal oxygen conditions, mice exposed to intermittent hypoxia experienced a substantially higher risk of death. The team observed multiple signs consistent with accelerated cardiac ageing, including:

- Raised blood pressure
- Impaired systolic and diastolic (pumping and filling) heart function
- Reduced blood-vessel flexibility (vascular stiffening)
- Lower coronary (heart) reserve
- Abnormalities in the heart's electrical activity (ECG changes)
Compared to controls, IH (intermittent hypoxia) mice exhibited higher mortality, elevated blood pressure, impaired systolic and diastolic function, vascular stiffening, reduced coronary reserve, and ECG abnormalities.
Implications
The findings support the view that chronic intermittent oxygen deprivation — as occurs in untreated obstructive sleep apnoea — imposes cumulative stress on the cardiovascular system that can reshape the heart's structure and function and potentially shorten lifespan.
Study authors emphasise the clinical importance of early diagnosis and treatment of sleep-disordered breathing. Common interventions include lifestyle changes, positional therapy, and continuous positive airway pressure (CPAP) therapy, which delivers pressurised air through a mask during sleep.
Although this research was performed in mice and direct translation to humans requires caution, the results reinforce existing concerns about the systemic effects of untreated sleep apnoea. The authors also call for improved screening and access to treatment, especially in rural and underserved communities where cardiovascular disease is often more prevalent and resources are limited.
Note: This article summarises a preclinical animal study. Patients with sleep problems should consult a healthcare professional for personalised advice and diagnosis.
Help us improve.