The FDA announced plans to remove its strongest "black box" warnings from many menopause hormone therapies, saying earlier risks have been overstated. HRT can relieve symptoms such as hot flashes, sleep disruption and cognitive fog, and newer lower‑dose or localized options are available. Critics argue the change was issued before broad consensus and warn that real risks remain; professional bodies say updated labels will help patients and clinicians make individualized decisions. The boxed warning for endometrial cancer on systemic estrogen‑only products will remain.
FDA to Remove Strongest Warnings from Many Menopause Hormone Therapies

US to remove strongest safety warnings from many menopause hormone therapies
The United States will remove the FDA's strongest safety warnings from many hormone therapies used to treat menopausal symptoms, officials announced Monday. Regulators said the risks linked to these therapies have been overstated in light of newer evidence and clearer guidance.
What is HRT and who it helps
Hormone replacement therapy (HRT) replaces estrogen that the body stops producing at menopause and is used to relieve symptoms such as hot flashes, brain fog, insomnia, night sweats and joint pain. Once commonly prescribed, HRT use declined worldwide after a landmark trial in the early 2000s associated certain formulations with increased risks.
Why the warnings are changing
That early trial—part of the Women’s Health Initiative—prompted so‑called "black box" warnings, the FDA's most prominent alert, highlighting possible links to specific cancers, cardiovascular events and a potential connection to dementia. Critics later noted that many participants were a decade or more past menopause and in their 60s, an age when cardiovascular risk rises independently of HRT.
Modern guidance generally identifies healthy, newly menopausal or perimenopausal people—typically in their 40s or 50s—as the most likely candidates to benefit from HRT. In addition, more localized and lower‑dose options are now available compared with older systemic formulations.
Reactions and debate
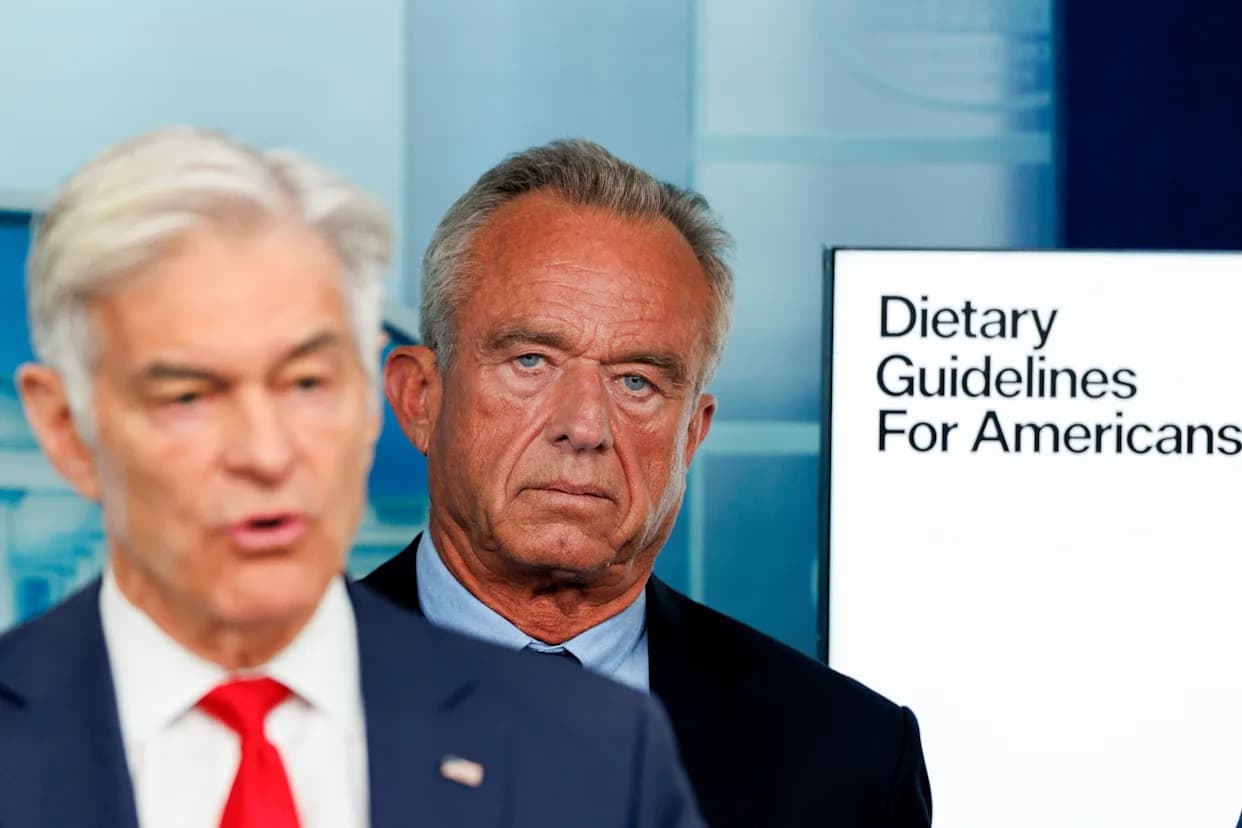
"We're challenging outdated thinking and recommitting to evidence‑based medicine that empowers rather than restricts," said Robert F. Kennedy Jr., who announced the measure. Many specialists had urged revisiting the black box label, arguing it can unduly alarm patients for whom benefits outweigh risks. Diana Zuckerman, president of the National Center for Health Research, said the warnings had become outdated but emphasized that "these products still have clear risks and the benefits are mostly for hot flashes and related symptoms of menopause, not for general health."
FDA chief Marty Makary rejected calls for a separate independent review panel, calling such committees "bureaucratic, long, often conflicted and very expensive." He had convened an expert panel over the summer that largely supported easing the label; some critics noted that a number of panel members had ties to pharmaceutical lobbying.
Adriane Fugh‑Berman of Georgetown University called the announcement premature and said changes normally follow broader scientific consensus. At the same time, professional groups such as the American College of Obstetricians and Gynecologists welcomed the move as an opportunity to improve patient–clinician shared decision‑making. Its president, Steven Fleischman, stressed the need to distinguish systemic estrogen (oral or patch) from low‑dose vaginal preparations and noted that systemic products carry risks that should be discussed individually.
What remains unchanged
The FDA said it will keep the boxed warning about endometrial cancer on systemic estrogen‑only products. Clinicians and patients are urged to discuss personal risk factors, benefits and alternatives when considering HRT, and experts call for continued high‑quality research to refine guidance.
Sarah Shealy, a nurse‑midwife and certified practitioner with the Menopause Society, welcomed the change and said it could improve access and education for people experiencing menopause.
Help us improve.